Introduction: Acute leukemias represent an important public health problem due to their high morbidity and mortality. Treatment failure due to abandonment or loss of follow-up (LOF) is a contributing factor to poor outcomes.
Objective: to determine the causes and outcomes of LOF in a cohort of adults with a diagnosis of acute leukemia and its impact on survival in a limited-resource setting.
Materials and Methods: We conducted a prospective, single-center cohort study from 2016 to 2022 in the university hospital; this institution is subsidized with funds from private and public sources. We included patients undergoing induction, consolidation, and maintenance phases of treatment for acute lymphoblastic (ALL) and acute myeloid leukemia (AML). LOF events were defined as discontinuation of follow-up beyond the last documented visit in the electronic medical records, with a timeframe of 2 to 4 weeks during the induction and 4 to 8 weeks in the consolidation or maintenance phases. Patients with LOF were contacted via telephone. Those who responded underwent a structured interview that assessed factors potentially contributing to the discontinuation of treatment. Treatment response, event-free survival (EFS), and overall survival (OS) in patients who lost follow-up were also assessed.
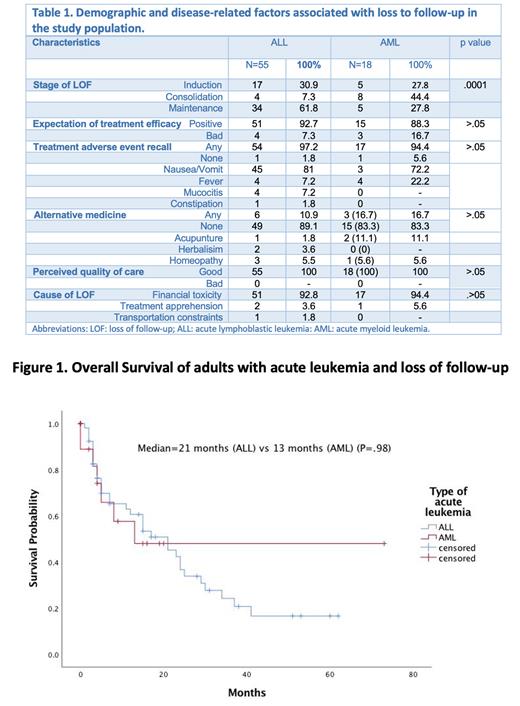
Results: From January 1, 2016, to October 31, 2022, a total of 391 patients were treated n=99 patients were found to have lost follow-up during first-line treatment, and 73 patients, (%) answered the phone call, 75.3% had been diagnosed with ALL, and 24.7% with AML. Of the 55 patients diagnosed with ALL, 52.7% were women, the median age was 26 years (range 18-86), and 96.4% were classified as a high-risk disease according to age, white blood cell count at diagnosis, CNS involvement, or steroid response. Most patients lived in an urban area (90.9%), and 74.5% didn't have healthcare coverage. Among the patients diagnosed with AML, 50% were male, the median age of diagnosis was 33 years (range 23-67), 94.4% resided in urban areas, and 83.3% of the patients did not have healthcare coverage, thus and molecular risk could not be determined due to the high cost of comprehensive genetic analysis. All patients were classified as low socioeconomic status, with a median income of $130 US dollars per month, (range, 81 -378 USD) for the ALL cohort and $180 USD for the AML group.
Based on the findings of the telephone survey, it was evident that economic constraints were the primary driver of treatment abandonment in both ALL and AML patients, accounting for 92.8% and 94.4% of cases, respectively. Specifically, 92.7% of the ALL group expressed difficulties in covering the costs of treatment, while 83.3% in the AML group faced similar challenges. For ALL patients LOF was more frequent during the maintenance phase, (61.8%) compared to consolidation in AML patients (44%).
Despite telephone contact, 76.4% of those with ALL and 77.8% of those with AML, could not continue follow-up. Concerning disease status, 11.1% of patients diagnosed with ALL and 34.5% of patients with AML that resumed follow-up after the phone call were diagnosed with relapsed disease. OS at 2 years from the time LOF was identified 49.1% for ALL and 61.1% for AML. Additionally, the 2-year EFS rates were 43.6% for ALL and 44.4% for AML.
Conclusions: Lack of access to financial resources and catastrophic healthcare expenditures were the main reason for abandoning treatment in patients with acute leukemia. Despite the loss of follow-up, the overall survival in both groups of patients showed favorable long-term outcomes; however, risk assessment strategies should be employed, and support programs implemented to improve outcomes in vulnerable populations.
Disclosures
Gomez-Almaguer:AMGEN: Consultancy, Honoraria; Janssen: Consultancy, Honoraria; Novartis: Honoraria; AbbVie: Consultancy, Honoraria. Gomez-De Leon:Astellas: Honoraria; Novartis: Honoraria; Abbvie: Honoraria; AMGEN: Honoraria; Jnssen: Other: Advisory board; Sanofi: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal